Vaccinologist Maurice Hilleman
Maurice Hilleman was a microbiologist, vaccinologist, inventor, and public health advocate of the 20th century. He developed several vaccines that are now given routinely to children and have increased the American lifespan by 30 years. However, he has received little recognition for his work, and few people know his name.
Hilleman received a scholarship to Montana State University, where he studied chemistry and microbiology. After graduating in 1941, he moved to the University of Chicago for doctoral work in microbiology. His thesis was on chlamydia, a common sexually-transmitted disease. At the time, it was believed that chlamydia was caused by a virus, but Hilleman discovered that it is caused by a bacterium and can be treated with antibiotics.
After receiving his PhD in 1944, Hilleman was expected to enter academia to research and teach. However, he decided to go to industry to learn industrial management and manufacture products. He described his rationale, “I wanted to do something. I wanted to make things!” He joined E. R. Squibb & Sons in New Brunswick, New Jersey, where he mass produced the influenza vaccine in chicken eggs, the same method used to make the annual flu vaccine today. Four years later, in 1948, Hilleman left for the Walter Reed Army Institute of Research in Washington, D.C. There, his task was to prevent the next influenza pandemic.
Seasonal influenza is the virus that we encounter every year. The virus is present year-round, but like many other respiratory diseases, cases peak in the colder months because the virus can spread between people more easily. As the virus multiplies in human cells, it undergoes random genetic changes caused by mistakes made by its copying enzyme. The more times the virus replicates, the more mistakes it can make. Most of these genetic changes have no effect, but some can make the virus look different. If enough changes accumulate, our immune systems have a harder time recognizing the virus and responding to it. That’s why immunity to the flu isn’t lifelong. However, the changes are small enough that immune systems can still remember the flu virus a little bit, providing at least some immunity.
Influenza can also undergo large genetic changes rapidly when multiple strains recombine into a hybrid virus. When this happens, the virus looks so different that our immune systems do not recognize it as the same virus. Many more people are infected by this drastically altered virus, and many more die. The virus can also spread rapidly through populations because people do not have immunity, causing a pandemic.
In early 1957, a strain of influenza began spreading in Hong Kong. Hilleman quickly realized that the cluster of several thousand cases could become a pandemic. One month after reading a New York Times article describing the epidemic, Hilleman obtained a sample of this influenza virus from a navy serviceman stationed in Asia. He injected the virus into a chicken egg and grew it in the membrane surrounding the embryo.
He tested antibodies from hundreds of Americans, both military servicemen and civilians, but none of the antibodies reacted to this new virus. He sent the sample to the World Health Organization, the U.S. Public Health Service, and the Commission on Influenza of the Armed Forces Epidemiological Board. All of them tested the sample against antibodies obtained from people around the world. Only a few antibody samples reacted to the virus, all of which were from elderly individuals. It is possible that they were exposed to a similar virus during their childhood, but no one younger had been exposed yet.
Hilleman knew that pre-existing immunity to the Hong Kong influenza strain was very low in the population, making conditions right for a pandemic. The only way to prevent it was to make a vaccine. Many scientists didn’t believe Hilleman’s claim that this influenza strain was significantly different from what was already circulating in humans. The U.S. military was reluctant to begin working on a new vaccine because the threat didn’t seem large enough. But Hilleman then sent the information out to pharmaceutical companies and convinced them to begin production. By July 1957, vaccines were being given out in the United States. By the end of the pandemic, more than 1 million people had died worldwide, with around 116,000 deaths in the USA. Hilleman is credited with averting a much higher death toll from the 1957 pandemic because of his rapid vaccine deployment.
These childhood diseases are not harmless; many children died before vaccines were available, and many die today because they lack access to vaccines. Some survivors sustain long term damage, particularly to the brain. Measles can cause pneumonia and encephalitis (brain swelling). Mumps frequently causes hearing loss, male infertility, and swelling of organs including the brain. Rubella, while relatively harmless to children, is deadly to fetuses in pregnant mothers infected with it. Polio paralyzes or kills many children. Chickenpox can attack the liver and brain, increase the risk of infection by certain deadly bacteria, and remain dormant in the body. Hepatitis can lead to lifelong liver dysfunction and eventually liver failure or cancer.
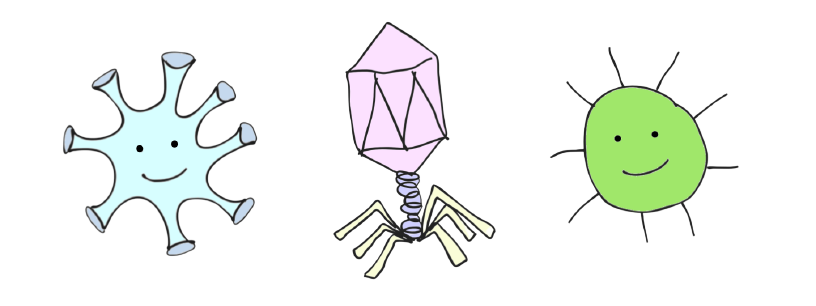
In late 1957, Hilleman left Walter Reed to become the director of virus and cell biology research at Merck & Co. in West Point, Pennsylvania. His ambitious goal at Merck was to make vaccines for all childhood diseases. Hilleman invented, improved, or manufactured 9 of the vaccines routinely given to children (6 viral, 3 bacterial), shown below. There are two dates of licensure for hepatitis B because two versions of the vaccine were made.
The viral vaccines that Hilleman made were all attenuated or inactivated. These methods either weaken (attenuate) the virus to make it less severe in humans or inactivate it to no longer be infectious. From his farm upbringing and influenza work at Walter Reed, Hilleman was well acquainted with chickens and how to grow viruses in eggs. Several human viruses, including influenza, can also infect chickens, and the membranes around the embryos in eggs replicate viruses very well.
Pathogens can be attenuated in several different ways. They can be grown at suboptimal temperatures or in different types of cells, or exposed to the elements to reduce their infectivity. French microbiologist Louis Pasteur was probably the first to develop attenuated vaccines. Along with scientists Charles Chamberland and Émile Roux, he made vaccines for rabies and anthrax. Pasteur dried out the spinal cords of rabbits that had died of rabies virus infection. The longer they were dried out, the weaker the virus became. To attenuate anthrax, Pasteur stored the bacteria at higher temperatures, making them less infectious.
To make his attenuated vaccines, Hilleman used a technique developed by South African-American virologist Max Theiler. Theiler created the yellow fever vaccine by repeatedly growing the deadly virus in mouse and chick embryos. He reasoned that over time, the virus would adapt to grow well in animal cells, while becoming worse at growing in human cells. When it is placed back in the human body, the virus is far less deadly, causing an immune reaction without disease. Theiler tested his vaccine in Brazilians at risk of contracting yellow fever. Most people developed antibodies, but nobody got sick from the vaccine. Theiler’s vaccine helped stop yellow fever epidemics in Brazil in the 1930s, and his vaccine is still in use today. 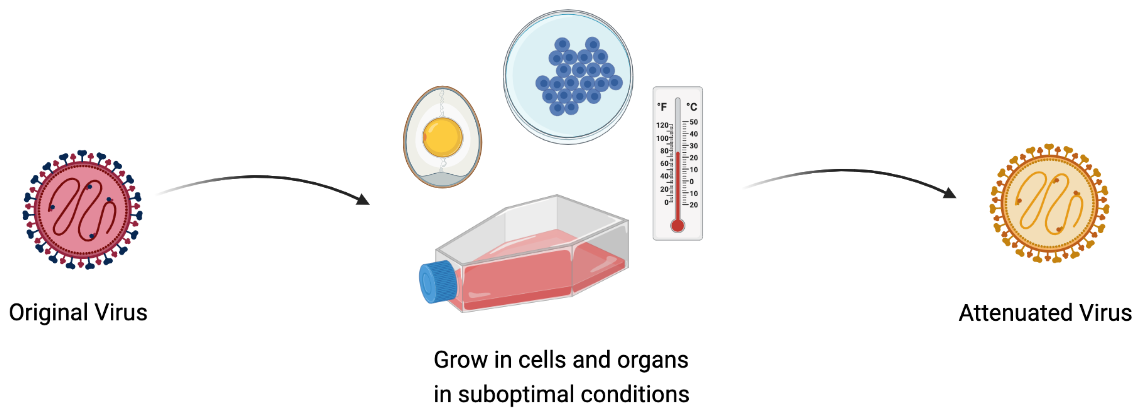
Hilleman and pediatrician Joseph Stokes Jr. gave Enders’ measles vaccine to children along with antibodies. The antibodies reduced the severity of side effects, but Hilleman was still not satisfied. He attenuated it further by passing it through chick embryo cells several more times. The final vaccine was licensed by Merck in 1968 and is the same vaccine given today. It doesn’t need to be given with antibodies. Today, the number of deaths from measles is around 200,000 per year worldwide. It used to be lower, but reduced vaccine coverage has increased cases.
Hilleman developed his mumps vaccine in the same way that he developed the pandemic influenza vaccine: by growing the virus repeatedly in chick embryos and cells to weaken it. The original virus was isolated from his older daughter Jeryl Lynn when she came down with a case of the mumps as a child in 1963. When Hilleman, Stokes, and another pediatrician, Robert Weibel, tested the vaccine in children in the Philadelphia area, they found a much lower incidence of mumps in vaccinated children than in the unvaccinated. The vaccine was licensed just four years later in 1967 and has since eliminated mumps in much of the developed world.

This image of Robert Weibel giving the mumps vaccine to Hilleman’s younger daughter, Kirsten, was used by Merck to promote the vaccine. Her older sister Jeryl, for whom the vaccine strain is named, offers comfort. It has since become an iconic photograph.
Hilleman developed an attenuated rubella virus vaccine by growing the virus in different animal cells and showed that it protected children from infection in 1965. However, he abandoned his vaccine at the request of philanthropist Mary Lasker in favor of another rubella vaccine being developed by government researchers Harry Meyer and Paul Parkman. Lasker believed that competition would slow down the process and that the government vaccine would be licensed more quickly. However, Hilleman further attenuated Meyer and Parkman's vaccine to reduce its side effects. He then had Merck produce millions of doses, helping avert an anticipated rubella epidemic in the early 1970s.
The rubella vaccine in use today was developed by physician Stanley Plotkin by growing the virus at low temperature. After Plotkin developed his better attenuated vaccine, Hilleman called him in 1978 to ask to begin producing doses at Merck for distribution. The risk of pregnancy complications after rubella infection in the first trimester - stillbirth, birth defects, or spontaneous abortion - is nearly 80%. But only one fetus has ever been harmed by the rubella vaccine given to the mother, demonstrating a remarkable safety profile.
After the 1960s, children were getting many shots to protect them from diseases. These are uncomfortable for children, and it is difficult for many parents to make repeated trips to a doctor's office. Hilleman mixed and stabilized the components of the measles, mumps, and rubella vaccines into one formulation, the MMR vaccine. After he showed that children who received MMR and children who received the 3 vaccines individually were equally protected from disease, the combination vaccine was licensed in 1971.
Chickenpox virus has a reputation for being a harmless childhood disease, but it can be deadly in some cases. A Japanese microbiologist, Michiaki Takahashi, developed the first chickenpox vaccine in the 1970s. He took fluid from the blister of a child with chickenpox, then grew it in different human and animal cells at low temperature. Hilleman further attenuated Takahashi’s virus strain and developed it into a vaccine that began to be used in the USA in 1995. 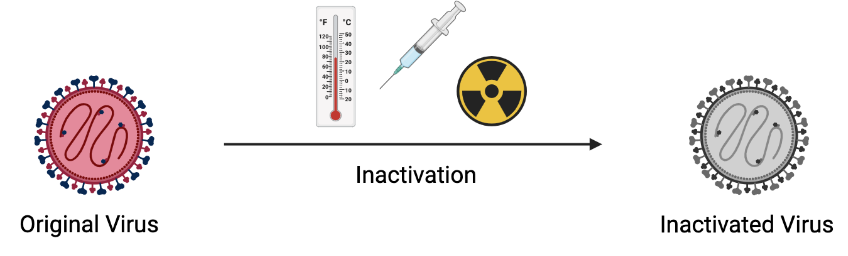
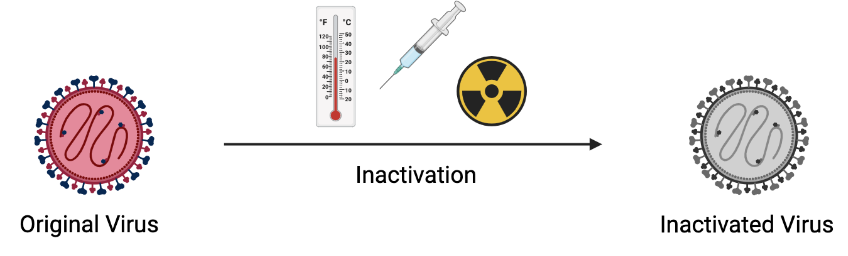
In the late 1970s, Hilleman obtained samples from the blood of homosexual men and injection drug users. These groups are at highest risk of getting hepatitis B because it is transmitted via sexual contact and blood. The blood Hilleman used also contained human immunodeficiency virus (HIV), which was not identified until the 1980s. However, the rigorous inactivation process he used destroyed HIV, along with hepatitis B and other viruses. Hilleman treated the samples with pepsin, urea, and formaldehyde.
Pepsin is a protein-destroying enzyme found in the body, and urea is a byproduct of metabolism found in urine (hence the name). Formaldehyde is used to inactivate other viruses like polio and influenza. With these 3 treatment steps, Hilleman aimed to destroy all proteins and viruses in the blood, except for the hepatitis B surface protein. This combination treatment was completely new, and Hilleman didn’t know with certainty whether hepatitis B surface protein had survived the process until he tested it in people. 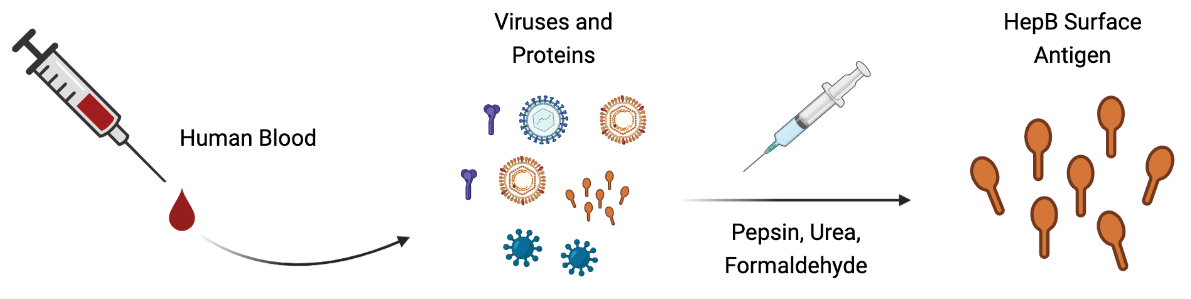
The invention of a new technique in molecular biology by Herbert Boyer and Stanley Cohen allowed for the hepatitis B vaccine to be produced without human blood. The two scientists combined their expertise to demonstrate that foreign genes could be inserted into bacteria or yeast. The microbes would then produce the desired protein. Hilleman and other Merck scientists capitalized on this to produce hepatitis B surface protein in yeast, rather than purifying it from blood. The resulting recombinant vaccine, not derived from human blood, was licensed in 1986. 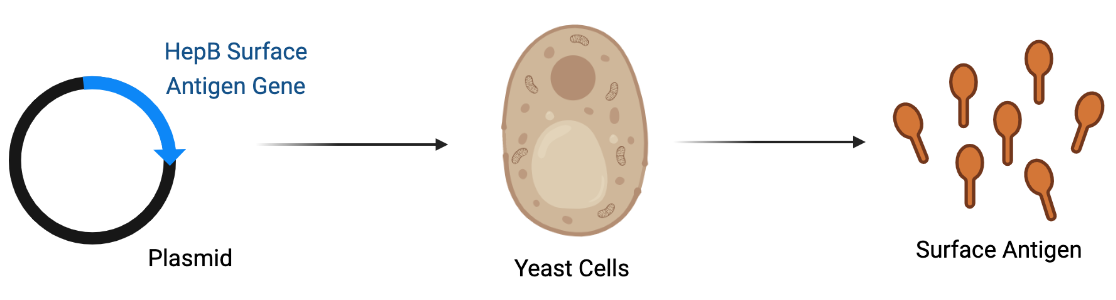
Although Hilleman didn’t invent these bacterial vaccines himself, his role in developing them and overseeing production was essential. Towards the end of the 20th century, fewer pharmaceutical companies wanted to produce vaccines. Maurice Hilleman was one of the few industry scientists who was eager to bring vaccines to market. Vaccines have to be developed into stable formulations and then mass produced, a herculean task itself. At Merck, he helped mass produce and make available the vaccines caused by the bacteria, Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae type b (Hib). He also updated the pneumococcal vaccine with more strains of bacteria to provide broader protection.
While at Walter Reed, Hilleman was sent to investigate a purported influenza outbreak among military recruits in Missouri. He discovered a new group of viruses, adenoviruses, which can cause flu-like symptoms in humans. Hilleman was also the first to purify and characterize interferon, a signaling protein made by your immune system in response to viruses. He found that animal cells produce interferon and that it helps fight viral infections.
At E.R. Squibb, Hilleman developed a vaccine for Japanese encephalitis. The virus is spread by mosquitoes and causes paralysis, coma, and death in one-third of individuals. During his PhD, Hilleman had discovered that the virus grows in mouse brains and could be inactivated with formaldehyde. He set up a production facility in a barn to produce the first Japanese encephalitis vaccine.
Hilleman also discovered an important monkey virus that helped advance our understanding of cancer. While he was attempting to make his own polio vaccine using monkey cells, Hilleman was concerned about contamination with monkey viruses. After several steps to remove or inactivate any viruses, Hilleman found that one virus had escaped. He called it simian virus 40 (SV40) because it was the 40th monkey virus to be discovered.
Frighteningly, when he injected the virus into laboratory animals, tumors formed throughout their bodies. Even worse, Hilleman found that both polio vaccines, which had already been given to millions of people, were contaminated with SV40. Over the next few years, Hilleman and others determined that SV40 did not cause cancer in humans and that the polio vaccines were safe. They were later made in human cells to eliminate the problem of monkey virus contamination. Although Hilleman discovered SV40, his name does not appear in one of the premier textbooks on cancer, written by Robert Weinberg, which discusses SV40 extensively.
While making his measles vaccine in the 1960s, a virus called chicken leukemia virus infected around 20% of all chickens in the United States. Around 80% of chickens infected with the virus developed various types of cancer, including leukemia and cancer of the liver, kidneys, and connective tissue. Human cells infected in the lab with the virus become cancerous, but it was unclear whether a person injected with the virus would develop cancer.
Hilleman didn’t take any chances with a potentially cancer-inducing virus in his vaccines. Because the leukemia virus was so common among chickens, he searched for a virus-free chicken flock. He eventually found one on a farm in Fremont, California, which he brought back to Merck to lay virus-free eggs in which to produce his vaccines. In 1972, it was determined that chicken leukemia virus does not cause cancer in humans. This was unknown when Hilleman made his egg-based vaccines, but he knew that he couldn’t risk contamination.
As a humble man, Hilleman did not put his name on any of the discoveries that he made. Many scientists name cell lines, mechanisms, theories, or phenomena after themselves, forever attaching their names to these discoveries. Hilleman named most of his vaccines after the source, strain number, or process used to generate them. The exception was his mumps vaccine, named after his daughter from whom it was isolated. But even so, it is called the Jeryl Lynn strain, with no reference to the surname Hilleman.
Another factor was his degree. Hilleman had a PhD, not an MD, so although he was instrumental in running field trials of his vaccines, the vaccines themselves were administered by doctors. These doctors were also the ones to discuss vaccines with parents and publish their trial findings, so in many cases, people believed the doctors had developed the vaccines.
As an industry scientist, Hilleman had greater anonymity than an academic scientist. Fair or not, the public had (and still has) the perception that industry scientists develop products for profit, while academic scientists conduct research for intellectual advancement. Hilleman and other vaccinologists had no intention of profiting from their life-saving vaccines, but this is how they were often seen. Hilleman was cognizant of the benefits of industry research - greater financial resources to focus on research and the ability to make products for people - and he chose this over academic prestige.
Even today, technological innovations from academic labs must be combined with industrial manufacturing capabilities to have a meaningful impact on human health. The COVID-19 vaccines developed by BioNTech, the National Institutes of Health, Harvard Medical School, and Oxford University could only be mass produced and distributed to people by pharmaceutical companies like Pfizer, Moderna, Johnson & Johnson, and AstraZeneca. Strong-willed Hilleman was often the bridge between academic scientists and the companies that manufactured vaccines.
Politicians, parents, personal injury lawyers, and others with little to no scientific or medical background claim without evidence that vaccines cause autism. No significant difference in autism rates has been found between vaccinated and unvaccinated children. Children are often diagnosed with autism around the same time they are receiving many vaccines, between 1 and 2 years of age, which is simply a coincidence. We also know that small quantities of thimerosal, a mercury-based preservative, in vaccines have no adverse effects on children. Thimerosal is even less hazardous than the environmental mercury that we are exposed to (i.e. from fish).
Vaccines are so effective that we forget that millions of people used to die of vaccine-preventable illnesses. It is difficult to predict who will have a mild infection and who will suffer lifelong complications or die, and vaccines protect everyone from taking that gamble. Vaccines reduce people’s need for treatment, reducing health care expenditure and allowing children to grow normally.
An ounce of prevention is worth a pound of cure. Even with improved medical care today, we are not immune to infectious diseases. More bacteria are becoming resistant to antibiotics. Hospitals operate dangerously close to capacity, so a surge of cases during an outbreak will push them over the edge. Many younger doctors are not familiar with diseases like mumps, diphtheria, and rubella because they were trained after vaccines were developed. If children constantly get sick from common diseases (even more than usual), parents will have to stay home to care for them, straining the workforce. And many disease survivors must live with long-term consequences. Measles, mumps, chickenpox, polio, rubella, and COVID-19 can cause permanent brain damage, paralysis, and organ dysfunction.
Hilleman lamented that the only way for the public to recognize the importance of childhood vaccines was to witness the suffering and death wrought by infectious diseases. We have seen more than a year of the health, economic, and psychological tolls of the COVID-19 pandemic, and even death and overwhelmed hospitals have not been enough to convince many people of the necessity of vaccines and infection control measures. Some amount of healthy skepticism of new drugs is necessary to ensure that they are rigorously tested. However, the data show that vaccines are safe in millions of people and reduce deaths and hospitalizations.
Hilleman was quick to give credit to others, and he recognized when they had produced a better product. He threw his weight behind others’ vaccines, helping mass produce them and get them to children because his ultimate goal was to help children, not take credit for himself. Tenacious, brilliant, driven, and compassionate, he worked to rid the world of childhood diseases. It is up to us now to continue that same work against the many new pathogenic microbes we will encounter.
For more information about Maurice Hilleman's life, check out a biography written by Paul Offit of the Children's Hospital of Philadelphia, Vaccinated: One Man's Quest to Defeat the World's Deadliest Diseases, and a documentary, Hilleman: A Perilous Quest to Save the World's Children.
Maurice Hilleman was born on August 30, 1919 in Miles City, Montana. He grew up on a farm and was the youngest in a family of 8 surviving children. His Lutheran family was deeply religious, but Hilleman was unsatisfied with the theological explanations given by church leaders about the natural world. He was fascinated by the evolutionary theories of Charles Darwin, encouraging an early love of science.
Hilleman received a scholarship to Montana State University, where he studied chemistry and microbiology. After graduating in 1941, he moved to the University of Chicago for doctoral work in microbiology. His thesis was on chlamydia, a common sexually-transmitted disease. At the time, it was believed that chlamydia was caused by a virus, but Hilleman discovered that it is caused by a bacterium and can be treated with antibiotics.
After receiving his PhD in 1944, Hilleman was expected to enter academia to research and teach. However, he decided to go to industry to learn industrial management and manufacture products. He described his rationale, “I wanted to do something. I wanted to make things!” He joined E. R. Squibb & Sons in New Brunswick, New Jersey, where he mass produced the influenza vaccine in chicken eggs, the same method used to make the annual flu vaccine today. Four years later, in 1948, Hilleman left for the Walter Reed Army Institute of Research in Washington, D.C. There, his task was to prevent the next influenza pandemic.
1957 Influenza Pandemic
Influenza ("the flu") is a notorious disease, but its ubiquity has made many people complacent about the damage it can do. The COVID-19 pandemic has been likened to the influenza pandemic of 1918-1919, but there have been several other influenza pandemics since then.
Seasonal influenza is the virus that we encounter every year. The virus is present year-round, but like many other respiratory diseases, cases peak in the colder months because the virus can spread between people more easily. As the virus multiplies in human cells, it undergoes random genetic changes caused by mistakes made by its copying enzyme. The more times the virus replicates, the more mistakes it can make. Most of these genetic changes have no effect, but some can make the virus look different. If enough changes accumulate, our immune systems have a harder time recognizing the virus and responding to it. That’s why immunity to the flu isn’t lifelong. However, the changes are small enough that immune systems can still remember the flu virus a little bit, providing at least some immunity.
Influenza can also undergo large genetic changes rapidly when multiple strains recombine into a hybrid virus. When this happens, the virus looks so different that our immune systems do not recognize it as the same virus. Many more people are infected by this drastically altered virus, and many more die. The virus can also spread rapidly through populations because people do not have immunity, causing a pandemic.
In early 1957, a strain of influenza began spreading in Hong Kong. Hilleman quickly realized that the cluster of several thousand cases could become a pandemic. One month after reading a New York Times article describing the epidemic, Hilleman obtained a sample of this influenza virus from a navy serviceman stationed in Asia. He injected the virus into a chicken egg and grew it in the membrane surrounding the embryo.
He tested antibodies from hundreds of Americans, both military servicemen and civilians, but none of the antibodies reacted to this new virus. He sent the sample to the World Health Organization, the U.S. Public Health Service, and the Commission on Influenza of the Armed Forces Epidemiological Board. All of them tested the sample against antibodies obtained from people around the world. Only a few antibody samples reacted to the virus, all of which were from elderly individuals. It is possible that they were exposed to a similar virus during their childhood, but no one younger had been exposed yet.
Hilleman knew that pre-existing immunity to the Hong Kong influenza strain was very low in the population, making conditions right for a pandemic. The only way to prevent it was to make a vaccine. Many scientists didn’t believe Hilleman’s claim that this influenza strain was significantly different from what was already circulating in humans. The U.S. military was reluctant to begin working on a new vaccine because the threat didn’t seem large enough. But Hilleman then sent the information out to pharmaceutical companies and convinced them to begin production. By July 1957, vaccines were being given out in the United States. By the end of the pandemic, more than 1 million people had died worldwide, with around 116,000 deaths in the USA. Hilleman is credited with averting a much higher death toll from the 1957 pandemic because of his rapid vaccine deployment.
Childhood Vaccines
The most notable contributions of Maurice Hilleman are the childhood vaccines he developed. In the 20th century, there were no treatments for diseases like measles, mumps, chickenpox, polio, diphtheria, pertussis (whooping cough), tuberculosis, and hepatitis. Even now, many of these diseases don’t have cures. Children simply had to wait out infections, surviving or succumbing. Death rates were high, and many children didn’t live past infancy, the time during which they are most susceptible to infections.
These childhood diseases are not harmless; many children died before vaccines were available, and many die today because they lack access to vaccines. Some survivors sustain long term damage, particularly to the brain. Measles can cause pneumonia and encephalitis (brain swelling). Mumps frequently causes hearing loss, male infertility, and swelling of organs including the brain. Rubella, while relatively harmless to children, is deadly to fetuses in pregnant mothers infected with it. Polio paralyzes or kills many children. Chickenpox can attack the liver and brain, increase the risk of infection by certain deadly bacteria, and remain dormant in the body. Hepatitis can lead to lifelong liver dysfunction and eventually liver failure or cancer.
In late 1957, Hilleman left Walter Reed to become the director of virus and cell biology research at Merck & Co. in West Point, Pennsylvania. His ambitious goal at Merck was to make vaccines for all childhood diseases. Hilleman invented, improved, or manufactured 9 of the vaccines routinely given to children (6 viral, 3 bacterial), shown below. There are two dates of licensure for hepatitis B because two versions of the vaccine were made.
| Vaccine | Year Licensed in the USA |
|---|---|
| Measles | 1963 |
| Mumps | 1967 |
| Rubella | 1969 |
| Meningococcus | 1974 |
| Pneumococcus | 1977 |
| Hepatitis B | 1981 / 1986 |
| Hib | 1987 |
| Hepatitis A | 1995 |
| Chickenpox | 1995 |
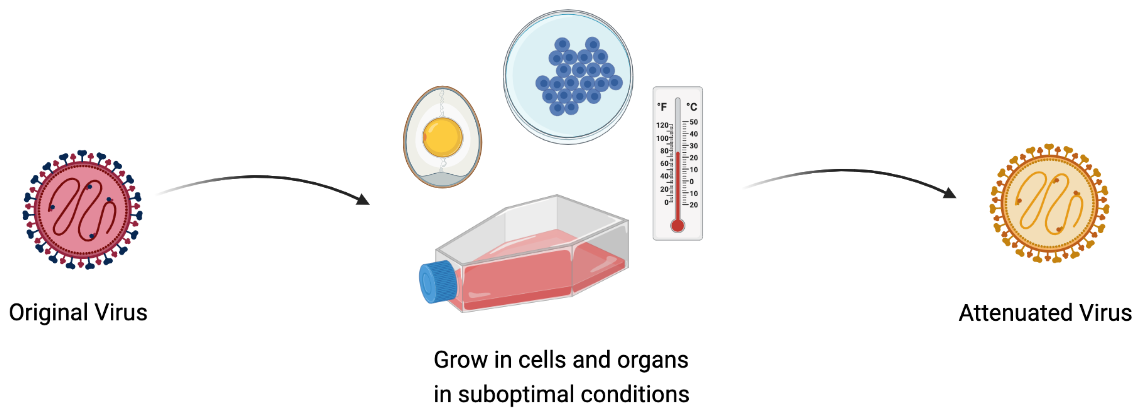
The viral vaccines that Hilleman made were all attenuated or inactivated. These methods either weaken (attenuate) the virus to make it less severe in humans or inactivate it to no longer be infectious. From his farm upbringing and influenza work at Walter Reed, Hilleman was well acquainted with chickens and how to grow viruses in eggs. Several human viruses, including influenza, can also infect chickens, and the membranes around the embryos in eggs replicate viruses very well.
Pathogens can be attenuated in several different ways. They can be grown at suboptimal temperatures or in different types of cells, or exposed to the elements to reduce their infectivity. French microbiologist Louis Pasteur was probably the first to develop attenuated vaccines. Along with scientists Charles Chamberland and Émile Roux, he made vaccines for rabies and anthrax. Pasteur dried out the spinal cords of rabbits that had died of rabies virus infection. The longer they were dried out, the weaker the virus became. To attenuate anthrax, Pasteur stored the bacteria at higher temperatures, making them less infectious.
To make his attenuated vaccines, Hilleman used a technique developed by South African-American virologist Max Theiler. Theiler created the yellow fever vaccine by repeatedly growing the deadly virus in mouse and chick embryos. He reasoned that over time, the virus would adapt to grow well in animal cells, while becoming worse at growing in human cells. When it is placed back in the human body, the virus is far less deadly, causing an immune reaction without disease. Theiler tested his vaccine in Brazilians at risk of contracting yellow fever. Most people developed antibodies, but nobody got sick from the vaccine. Theiler’s vaccine helped stop yellow fever epidemics in Brazil in the 1930s, and his vaccine is still in use today.
Measles, Mumps, Rubella, and Chickenpox
Hilleman developed attenuated vaccines for measles, mumps, and rubella in the 1960s. A research group at Boston Children’s Hospital led by John Enders had isolated measles virus and developed an attenuated vaccine by growing the virus in different cell types. But the vaccine frequently caused side effects like rash and high fever. When pharmaceutical companies like Merck began making Enders’ vaccine, Hilleman, who was always devoted to making vaccines safe and effective, decided to improve it.
Hilleman and pediatrician Joseph Stokes Jr. gave Enders’ measles vaccine to children along with antibodies. The antibodies reduced the severity of side effects, but Hilleman was still not satisfied. He attenuated it further by passing it through chick embryo cells several more times. The final vaccine was licensed by Merck in 1968 and is the same vaccine given today. It doesn’t need to be given with antibodies. Today, the number of deaths from measles is around 200,000 per year worldwide. It used to be lower, but reduced vaccine coverage has increased cases.
Hilleman developed his mumps vaccine in the same way that he developed the pandemic influenza vaccine: by growing the virus repeatedly in chick embryos and cells to weaken it. The original virus was isolated from his older daughter Jeryl Lynn when she came down with a case of the mumps as a child in 1963. When Hilleman, Stokes, and another pediatrician, Robert Weibel, tested the vaccine in children in the Philadelphia area, they found a much lower incidence of mumps in vaccinated children than in the unvaccinated. The vaccine was licensed just four years later in 1967 and has since eliminated mumps in much of the developed world.

This image of Robert Weibel giving the mumps vaccine to Hilleman’s younger daughter, Kirsten, was used by Merck to promote the vaccine. Her older sister Jeryl, for whom the vaccine strain is named, offers comfort. It has since become an iconic photograph.
Hilleman developed an attenuated rubella virus vaccine by growing the virus in different animal cells and showed that it protected children from infection in 1965. However, he abandoned his vaccine at the request of philanthropist Mary Lasker in favor of another rubella vaccine being developed by government researchers Harry Meyer and Paul Parkman. Lasker believed that competition would slow down the process and that the government vaccine would be licensed more quickly. However, Hilleman further attenuated Meyer and Parkman's vaccine to reduce its side effects. He then had Merck produce millions of doses, helping avert an anticipated rubella epidemic in the early 1970s.
The rubella vaccine in use today was developed by physician Stanley Plotkin by growing the virus at low temperature. After Plotkin developed his better attenuated vaccine, Hilleman called him in 1978 to ask to begin producing doses at Merck for distribution. The risk of pregnancy complications after rubella infection in the first trimester - stillbirth, birth defects, or spontaneous abortion - is nearly 80%. But only one fetus has ever been harmed by the rubella vaccine given to the mother, demonstrating a remarkable safety profile.
After the 1960s, children were getting many shots to protect them from diseases. These are uncomfortable for children, and it is difficult for many parents to make repeated trips to a doctor's office. Hilleman mixed and stabilized the components of the measles, mumps, and rubella vaccines into one formulation, the MMR vaccine. After he showed that children who received MMR and children who received the 3 vaccines individually were equally protected from disease, the combination vaccine was licensed in 1971.
Chickenpox virus has a reputation for being a harmless childhood disease, but it can be deadly in some cases. A Japanese microbiologist, Michiaki Takahashi, developed the first chickenpox vaccine in the 1970s. He took fluid from the blister of a child with chickenpox, then grew it in different human and animal cells at low temperature. Hilleman further attenuated Takahashi’s virus strain and developed it into a vaccine that began to be used in the USA in 1995.
Viral Hepatitis
Hepatitis viruses are a group of unrelated viruses that attack the liver. There are 5 distinct types that infect humans, and Hilleman developed vaccines for hepatitis A and B (the vaccine for hepatitis B also protects against hepatitis D).
Hepatitis B (HepB) is the more dangerous of the two because it can cause lifelong (chronic) infection. Around 350 million people are chronically infected today, and 800,000-900,000 die each year from liver failure and cancer. Before Hilleman, scientists Baruch Bloomberg, Alfred Prince, and Saul Krugman had identified hepatitis B virus, its surface protein, and that antibodies to the surface protein protected children from getting the disease. Based on this knowledge, Hilleman decided to make a vaccine using the surface protein.
In the late 1970s, Hilleman obtained samples from the blood of homosexual men and injection drug users. These groups are at highest risk of getting hepatitis B because it is transmitted via sexual contact and blood. The blood Hilleman used also contained human immunodeficiency virus (HIV), which was not identified until the 1980s. However, the rigorous inactivation process he used destroyed HIV, along with hepatitis B and other viruses. Hilleman treated the samples with pepsin, urea, and formaldehyde.
Pepsin is a protein-destroying enzyme found in the body, and urea is a byproduct of metabolism found in urine (hence the name). Formaldehyde is used to inactivate other viruses like polio and influenza. With these 3 treatment steps, Hilleman aimed to destroy all proteins and viruses in the blood, except for the hepatitis B surface protein. This combination treatment was completely new, and Hilleman didn’t know with certainty whether hepatitis B surface protein had survived the process until he tested it in people.
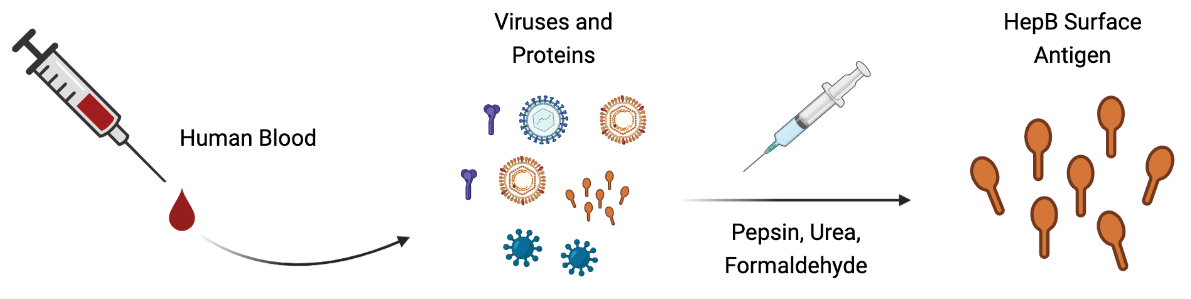
Many people were hesitant to receive the vaccine because it was derived from blood, though it didn't contain blood itself. Hilleman eventually persuaded Merck executives and colleagues to take it, and no one developed hepatitis in the first 6 months, suggesting that it was safe. Next, he had to study its efficacy. He worked with Wolf Szmuness to study the vaccine in 1000 homosexual men in New York City. Those who received the vaccine were 75% less likely to get hepatitis B than those who did not get the vaccine. The vaccine was licensed in 1981. However, the discovery of HIV and the horrific disease it causes, AIDS, intensified worries over Hilleman’s vaccine, even though he had demonstrated that no virus survived his inactivation process.
The invention of a new technique in molecular biology by Herbert Boyer and Stanley Cohen allowed for the hepatitis B vaccine to be produced without human blood. The two scientists combined their expertise to demonstrate that foreign genes could be inserted into bacteria or yeast. The microbes would then produce the desired protein. Hilleman and other Merck scientists capitalized on this to produce hepatitis B surface protein in yeast, rather than purifying it from blood. The resulting recombinant vaccine, not derived from human blood, was licensed in 1986.
Hepatitis A is a food-borne infection that is common in areas with poor sanitation where sewage and drinking water can mix. Hilleman grew hepatitis A virus in human fetal cells, attenuated it by growing it at lower-than-normal body temperature, and then inactivated it with formaldehyde. The attenuation step was just for added safety. The vaccine was tested in a community of Orthodox Jews just outside of New York City. The community was chosen because many children of different ages lived in close proximity, allowing hepatitis A to spread quickly. Pediatrician Alan Werzberger conducted a trial in 1000 children. Hilleman’s vaccine prevented hepA infection in 100% of vaccinated children, and it was licensed in 1995.
Bacterial Vaccines
Vaccines for bacterial infections are typically more difficult to develop than those for viral infections. Although bacteria were discovered earlier because they are larger, bacteria contain far more proteins than viruses, and it is difficult to determine which bacterial proteins will induce a protective immune response.
Although Hilleman didn’t invent these bacterial vaccines himself, his role in developing them and overseeing production was essential. Towards the end of the 20th century, fewer pharmaceutical companies wanted to produce vaccines. Maurice Hilleman was one of the few industry scientists who was eager to bring vaccines to market. Vaccines have to be developed into stable formulations and then mass produced, a herculean task itself. At Merck, he helped mass produce and make available the vaccines caused by the bacteria, Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae type b (Hib). He also updated the pneumococcal vaccine with more strains of bacteria to provide broader protection.
Other Contributions
Hilleman also developed an important vaccine for chickens. Marek’s disease is found in nearly every chicken flock in the world, causing paralysis and many cancers. Because it is highly infectious and not treatable, farmers simply kill infected birds. Hilleman obtained a sample of a related virus from turkeys and developed it into a vaccine for chickens. He found a flock of chickens in New Hampshire known for its supreme egg laying, meat production, and susceptibility to Marek’s disease. He convinced Merck to buy the farm in 1974, and soon, the company was producing chickens and eggs from the vaccinated flock. The price of chicken meat plummeted because of increased chicken survival.
While at Walter Reed, Hilleman was sent to investigate a purported influenza outbreak among military recruits in Missouri. He discovered a new group of viruses, adenoviruses, which can cause flu-like symptoms in humans. Hilleman was also the first to purify and characterize interferon, a signaling protein made by your immune system in response to viruses. He found that animal cells produce interferon and that it helps fight viral infections.
At E.R. Squibb, Hilleman developed a vaccine for Japanese encephalitis. The virus is spread by mosquitoes and causes paralysis, coma, and death in one-third of individuals. During his PhD, Hilleman had discovered that the virus grows in mouse brains and could be inactivated with formaldehyde. He set up a production facility in a barn to produce the first Japanese encephalitis vaccine.
Hilleman also discovered an important monkey virus that helped advance our understanding of cancer. While he was attempting to make his own polio vaccine using monkey cells, Hilleman was concerned about contamination with monkey viruses. After several steps to remove or inactivate any viruses, Hilleman found that one virus had escaped. He called it simian virus 40 (SV40) because it was the 40th monkey virus to be discovered.
Frighteningly, when he injected the virus into laboratory animals, tumors formed throughout their bodies. Even worse, Hilleman found that both polio vaccines, which had already been given to millions of people, were contaminated with SV40. Over the next few years, Hilleman and others determined that SV40 did not cause cancer in humans and that the polio vaccines were safe. They were later made in human cells to eliminate the problem of monkey virus contamination. Although Hilleman discovered SV40, his name does not appear in one of the premier textbooks on cancer, written by Robert Weinberg, which discusses SV40 extensively.
Hilleman’s Commitment to Vaccine Safety
The anti-vaccine movement has stirred up uncertainty about the safety and efficacy of various vaccines. Most of the sources cited have been discredited, and the diseases themselves are far worse than any side effects of the vaccines. Before becoming commercially available, vaccines go through a rigorous testing process to ensure that they are safe and effective. Regulatory agencies like the Food and Drug Administration have much more oversight now than they did decades ago. Even so, Maurice Hilleman was dedicated to testing the safety and efficacy of his vaccines himself. Unsatisfied with the harsh side effects of the measles and rubella vaccines developed by others, he attenuated them further to make them safer.
While making his measles vaccine in the 1960s, a virus called chicken leukemia virus infected around 20% of all chickens in the United States. Around 80% of chickens infected with the virus developed various types of cancer, including leukemia and cancer of the liver, kidneys, and connective tissue. Human cells infected in the lab with the virus become cancerous, but it was unclear whether a person injected with the virus would develop cancer.
Hilleman didn’t take any chances with a potentially cancer-inducing virus in his vaccines. Because the leukemia virus was so common among chickens, he searched for a virus-free chicken flock. He eventually found one on a farm in Fremont, California, which he brought back to Merck to lay virus-free eggs in which to produce his vaccines. In 1972, it was determined that chicken leukemia virus does not cause cancer in humans. This was unknown when Hilleman made his egg-based vaccines, but he knew that he couldn’t risk contamination.
Lack of Recognition
Despite his immense impact on childhood infections and human life expectancy, few people know that Maurice Hilleman was the person behind so many of the vaccines we take for granted. Even among infectious disease specialists and pediatricians, he is not nearly as well known as Jonas Salk and Albert Sabin, the developers of the two polio vaccines.
As a humble man, Hilleman did not put his name on any of the discoveries that he made. Many scientists name cell lines, mechanisms, theories, or phenomena after themselves, forever attaching their names to these discoveries. Hilleman named most of his vaccines after the source, strain number, or process used to generate them. The exception was his mumps vaccine, named after his daughter from whom it was isolated. But even so, it is called the Jeryl Lynn strain, with no reference to the surname Hilleman.
Another factor was his degree. Hilleman had a PhD, not an MD, so although he was instrumental in running field trials of his vaccines, the vaccines themselves were administered by doctors. These doctors were also the ones to discuss vaccines with parents and publish their trial findings, so in many cases, people believed the doctors had developed the vaccines.
As an industry scientist, Hilleman had greater anonymity than an academic scientist. Fair or not, the public had (and still has) the perception that industry scientists develop products for profit, while academic scientists conduct research for intellectual advancement. Hilleman and other vaccinologists had no intention of profiting from their life-saving vaccines, but this is how they were often seen. Hilleman was cognizant of the benefits of industry research - greater financial resources to focus on research and the ability to make products for people - and he chose this over academic prestige.
Even today, technological innovations from academic labs must be combined with industrial manufacturing capabilities to have a meaningful impact on human health. The COVID-19 vaccines developed by BioNTech, the National Institutes of Health, Harvard Medical School, and Oxford University could only be mass produced and distributed to people by pharmaceutical companies like Pfizer, Moderna, Johnson & Johnson, and AstraZeneca. Strong-willed Hilleman was often the bridge between academic scientists and the companies that manufactured vaccines.
Vaccines and the Future
Towards the end of his life, Hilleman witnessed the rise of the anti-vaccine movement. Fueled by false claims, insufficient data, and a forgetfulness of the devastation of infectious diseases, the movement has led to outbreaks of diseases like measles, pertussis, hepatitis A, and meningococcus that Hilleman and other scientists’ vaccines had come close to eliminating.
Politicians, parents, personal injury lawyers, and others with little to no scientific or medical background claim without evidence that vaccines cause autism. No significant difference in autism rates has been found between vaccinated and unvaccinated children. Children are often diagnosed with autism around the same time they are receiving many vaccines, between 1 and 2 years of age, which is simply a coincidence. We also know that small quantities of thimerosal, a mercury-based preservative, in vaccines have no adverse effects on children. Thimerosal is even less hazardous than the environmental mercury that we are exposed to (i.e. from fish).
Vaccines are so effective that we forget that millions of people used to die of vaccine-preventable illnesses. It is difficult to predict who will have a mild infection and who will suffer lifelong complications or die, and vaccines protect everyone from taking that gamble. Vaccines reduce people’s need for treatment, reducing health care expenditure and allowing children to grow normally.
An ounce of prevention is worth a pound of cure. Even with improved medical care today, we are not immune to infectious diseases. More bacteria are becoming resistant to antibiotics. Hospitals operate dangerously close to capacity, so a surge of cases during an outbreak will push them over the edge. Many younger doctors are not familiar with diseases like mumps, diphtheria, and rubella because they were trained after vaccines were developed. If children constantly get sick from common diseases (even more than usual), parents will have to stay home to care for them, straining the workforce. And many disease survivors must live with long-term consequences. Measles, mumps, chickenpox, polio, rubella, and COVID-19 can cause permanent brain damage, paralysis, and organ dysfunction.
Hilleman lamented that the only way for the public to recognize the importance of childhood vaccines was to witness the suffering and death wrought by infectious diseases. We have seen more than a year of the health, economic, and psychological tolls of the COVID-19 pandemic, and even death and overwhelmed hospitals have not been enough to convince many people of the necessity of vaccines and infection control measures. Some amount of healthy skepticism of new drugs is necessary to ensure that they are rigorously tested. However, the data show that vaccines are safe in millions of people and reduce deaths and hospitalizations.
A Scientist for the Ages
After mandatory retirement from Merck at age 65, he became the director of the newly created Merck Institute for Vaccinology, and for the next 20 years, he wrote review articles and opinion pieces and advised many other scientists. Ever the experimentalist, he was attempting a cancer vaccine on himself when he died of cancer on April 11, 2005.
Hilleman was quick to give credit to others, and he recognized when they had produced a better product. He threw his weight behind others’ vaccines, helping mass produce them and get them to children because his ultimate goal was to help children, not take credit for himself. Tenacious, brilliant, driven, and compassionate, he worked to rid the world of childhood diseases. It is up to us now to continue that same work against the many new pathogenic microbes we will encounter.
For more information about Maurice Hilleman's life, check out a biography written by Paul Offit of the Children's Hospital of Philadelphia, Vaccinated: One Man's Quest to Defeat the World's Deadliest Diseases, and a documentary, Hilleman: A Perilous Quest to Save the World's Children.
Leave a Comment